Skeletal data provide the most direct evidence of the health status and disease burden of past populations. The amount of trauma a population was subject to can be studied in the number and distribution of fractures and Schmorl's nodes, both of which are readily studied in dry bone. Much less easy to assess are the acute, infectious diseases from which many of the population probably died such as cholera, typhus, bubonic plague and influenza, as these either kill or are resolved before changes to the bones develop. Diseases that show up on the bones are generally chronic, such as tuberculosis, leprosy, syphilis and bone infections. Unfortunately, the responses that a bone can make to a disease stimulus are limited and so different diseases may produce similar bony pictures. In addition, many of the techniques that aid diagnosis in modern medicine, such as blood tests, are unavailable when dealing with dry bone, and so diagnoses can rarely be precise or unequivocal.
Fractures
Analysis of the type and distribution of fractures within and between populations may elucidate aspects of lifestyle. It should be noted that fractures suffered at or close to death may be difficult or impossible to distinguish from post-mortem breaks. Evidence of partial (greenstick) fractures sustained during childhood may be completely remodelled and undetectable if the individual survived to adulthood.
Seventeen individuals suffered at least one fracture, twelve being male and all being adult. Twenty percent (12/60) of males and nine percent (4/46) of females displayed at least one fracture, although this figure is probably an underestimate as many skeletons were incomplete. Males were three times more likely to be affected than females.
Three individuals, all males, suffered fractures of more than one 'region' (fracture of the tibia is often associated with that of the fibula, the lower leg thus being scored as one region). The ribs, left tibia and fibula and left clavicle were fractured in SK 211, the right clavicle and a rib in SK 255 and the right radius, left second metatarsal head and right third metacarpal shaft in SK 259.
Additional long bone shaft fractures include those of the tibia and/or fibula (SK 223, male, possible leper, Tibia 67), ulna (SK 234, female) , rib (SK 239, male, associated with a number of other injuries), distal fibula (SK 252), adult of indeterminate sex, ununited fracture), phalanges of the foot (SK 262, female) and two distal radii (Colles' fracture, usually seen in post-menopausal women and often being caused by a fall onto the outstretched hand; Wiles 1960).
At least three fractures of the articular surface were noted. One male (SK 221) displayed a fracture of the proximal facet of the first metacarpal possibly caused by a blow or falling onto the clenched fist. One Colles fracture of the radius involved the distal articular surface and was associated with secondary degenerative changes at this joint. The shaft fracture of Tibia 67 (see data) was associated with a hair-line fracture of the distal articular surface.
Most fractures had healed soundly and in good alignment. However, a small number of possible ununited fractures was noted. The distal tip of the fibula of SK 252 was separate from the shaft, the two parts fitting neatly together, although slight movement between elements was indicated by slight eburnation of the fractured surfaces. Re-union may have been prevented by the inhibiting effects of joint fluid (Hutchison pers. comm.). However, the bone is very neatly and cleanly separated on a horizontal plane, unusual for a fracture, and the diagnosis remains uncertain. An alternative explanation may be of an unusual accessory, unfused epiphysis.
A tentative diagnosis of avulsion fracture with non-union was made in two further cases. The tuberosity of the left fifth metatarsal of SK 258 (middle aged female) and the right navicular tuberosity of SK 259 (old adult male) were missing, the affected areas being flat and pitted. Avulsion injuries to these bones are caused by forcible inversion and eversion of the foot respectively (Wiles 1960), although avulsion of the navicular tuberosity is uncommon in modern practice. Similar lesions of the fifth metatarsal were seen at Whithorn (Cardy 1997a), and similar lesions of the navicular at both Cirencester (Wells 1982, 188) and Whithorn (Cardy 1997a). These bones have not been included in the fracture frequencies quoted above.
Fractures were most common in the fibula followed by the clavicle, both bones that are commonly fractured in modern populations, the fibula because of its exposed position on the outside of the lower leg and the clavicle which tends to be broken during falls onto the outstretched arm.
Fractures were assessed for most probable cause. Spiral fractures and avulsion fractures were considered most likely to have been caused by indirect, accidental violence, whilst transverse fractures including parry fractures (associated with raising the arm to ward off a blow) were considered to result from direct violence, which may or may not have been deliberate. Most, if not all of the fractures in the present group could have been the result of indirect trauma. One parry fracture was noted (female, SK 234). Unambiguous evidence of interpersonal violence, however, was seen in the cranial injuries. There was no evidence of infection associated with fracture, suggesting that most fractures were closed.
The type and distribution of fractures was normal (Table 27), the two most vulnerable bones being fractured most often. The predominance of fractures in males seen in Aberdeen has been noted in many other archaeological groups including Linlithgow (Cross and Bruce 1989); Kirkhill, St Andrews (Bruce et al. 1990); Logies Lane, St Andrews (Cardy 1997b); Whithorn (Cardy 1997a); Cirencester (Wells 1982) and St Helen-on-the-Walls, York (Dawes 1980)). This no doubt reflects lifestyle differences and the sexual division of labour. Most fractures appear to have been caused during the course of everyday life with little evidence of violent interactions. Most healed well and in good alignment.
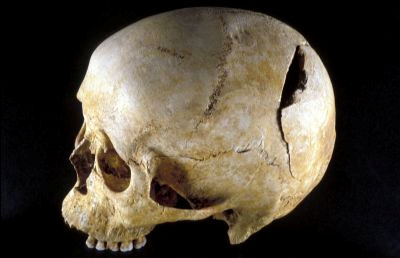
Cranial injury
A number of cranial injuries were evident, at least one of which indicates interpersonal violence. SK 239, an early middle aged male, was relatively complete and well preserved. There were a number of conditions of note throughout the skeleton, the most significant being a cleanly struck, unhealed blade wound to the left parietal [Photo 0316], 85mm in diameter. The characteristics of the injury indicate that the weapon must have been strong, thin and sharp, perhaps being something like a meat cleaver (J. Grieve, pers. comm.). Whilst the wound would have bled profusely, it need not have been fatal as the injury was open and therefore unlikely to have caused the increase in intracranial pressure which is one of the greatest dangers of head injuries (P. Johnston, pers. comm.). A small, clean, unhealed lesion of the right humeral shaft was also noted, apparently caused while the arm was held over the head, perhaps in an attempt to ward off a blow. It seems likely both injuries were caused by the same weapon. Perhaps most interestingly, there is a series of closely aligned scores alongside the cranial wound, possibly caused by an attempt to remove a piece of loose bone. The treatment, however, was unsuccessful, and the individual died soon after. Other indicators of past trauma noted on this individual include spondylolysis of the 5th lumbar vertebra, three fractured ribs, avulsion injury of the left patella caused by severe trauma to the quadriceps or rectus femoris and severe secondary joint disease of the first joint of the left first finger. There was also bilateral medial bowing of the second to fifth metatarsals, perhaps caused by habitually wearing tight footwear from childhood, and pronounced development of the attachments of the flexors and extensors of the forearm on the humerus. These features contribute to a picture of a physically active individual, exposed to traumatic injury on more than one occasion, the last of which caused his death.
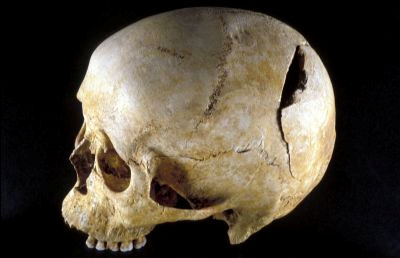
The cranium of a mature adult male (CR 6) [Photo 0027] displayed an oval, flat lesion of the right frontal which measured 60mm x 47mm. The injury may have been caused by a tangential blow from a heavy blade but is unlikely to have contributed to death as it is very well healed. Differential diagnoses include a benign soft tissue tumour which caused remodelling of the underlying bone (J. Grieve, pers. comm.).

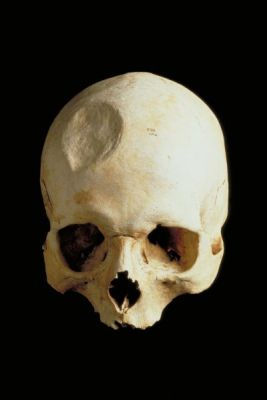
Two cranial compression fractures were noted. One calvarium (CR 14, young adult, possible female) displayed a depressed injury measuring approximately 45mm x 35mm in the right fronto-temporal region with a corresponding bulge on the inner surface. The bone thinned towards the centre of the injury which may indicate that part of the wound was covered only by fibrous tissue, although post-mortem damage precludes definitive conclusions. The wound was well-healed, and was unlikely to have contributed to death. A similar, but less severe injury was seen on the left frontal of a second disarticulated cranium [Photo 0030] (CR 13, adult of indeterminate sex). The compressed area measured 18mm by 15mm and a small, corresponding bulge [Photo 0278] was noted on the inner surface. Again, this injury healed well and was unlikely to have contributed to death.

Other cranial injuries include a possible blade injury (SK 41) and a possible healed trephination of a disarticulated calvarium, originally designated SK 111.
Schmorl's nodes
Schmorl's nodes are pits or depressions on the surface of the vertebral body caused by herniation of the intervertebral disc material into the bone, usually during adolescence or young adulthood while the intervertebral disc is still turgid. The nodes develop in response to trauma, usually thought to be of a sudden, compressive nature such as heavy lifting. The clinical significance of the nodes is unclear as they may be asymptomatic in the living.
Each Schmorl's node was recorded pictorially and a grade of severity from 1 (slight) to 3 (severe) assigned. Frequencies of affected individuals were determined for SKs with thoracic spines that were largely complete between the 6th-12th thoracic vertebra and with four of the five lumbar vertebrae present. Schmorl's nodes were noted in 46 adults (18 females; 28 males) but no immatures. Eighty three percent (10/12) of females and 91% of males (21/23) with both thoracic and lumbar spines displayed Schmorl's nodes (Table 28, Table 29).
Sex differences in the frequency of Schmorl's nodes (Table 30) appear to have been greatest in London and least in the eastern Scottish groups with south-west Scotland in an intermediate position. St John's Tower, Ayr on the west coast stands out in a reversal of the expected pattern, with more females than males being affected. This group displayed other, similar reversals, although the sample size was unfortunately small (48 individuals). Such variation is tantalising, indicating different factors operating between the sexes in different societies, both regional and temporal, which may reflect differences in lifestyle. Unfortunately the development of Schmorl's nodes is incompletely understood and interpretation is difficult, although it seems very likely that groups in which they are more frequent were more subject to physical stresses.
Intervertebral osteochondrosis
Osteochondrosis of the spine is manifest as semi-circular lytic lesions of the anterior part of the vertebral body, usually in the lower thoracic and lumbar regions. Resnick and Niwayama (1978) suggest that multiple Schmorl's nodes in early life may lead to this disorder and Kelley (1982) suggests that intervertebral osteochondritis is related to physical stress, probably during the second and third decades of life. In older individuals the lesions may become indistinguishable from other degenerative changes. This condition was noted in one late middle-aged female (SK 212) in the present sample. The 5th and 7th-8th thoracic vertebrae and the 2nd-5th lumbar vertebrae were affected. Neither the number nor nature of lesions in this group was remarkable.
Spondylolysis
This condition is manifest as separation of the vertebral body and superior facet joints from the inferior facet joints via the pars interarticularis. The precise aetiology is unknown, although stress such as repeated, forced extension of the spine would appear to be largely responsible, although there is a familial tendency towards the condition. The defect was not demonstrated in the studies of foetal or neonatal material reviewed by El-Najar and McWilliams (1978), and appears clinically between the ages of seven and twenty years, when perhaps five percent of the population may be affected (Hensinger 1990). Certain segments of the population are especially prone to the condition including gymnasts (Jackson et al. 1976), rowers, soldiers carrying heavy backpacks and interior linesmen, where up to 50% of individuals may be affected (Ferguson et al. 1974). The lesion was absent from a group of 125 non-ambulatory adults (Rosenberg 1981). Spondylolysis may be asymptomatic, especially in the young, or it may cause chronic low back pain and spinal stenosis (narrowing) if the defective vertebral body slips forward (Eisenstein 1978). These symptoms are probably consequent upon degenerative changes associated with the condition and nerve root compression. The fifth lumbar vertebra is affected in 85% of cases (Hresko and Micheli 1990).
Spondylolysis was noted in five adult males and one adult female. The fifth lumbar vertebra was involved in each case, giving a frequency of 9% (6/66). The predominance in males indicates greater stresses imposed on the male lumbar spine. The spatial distribution of those with spondylolysis was examined and no groupings found.
Enthesopathies
Bony outgrowths known as enthesopathies may develop in response to stress in areas where the tendons or ligaments are attached to the bone. These markers may record a single, high level episode or repeated minor episodes. They are also associated with diffuse idiopathic skeletal hyperostosis (DISH), a benign condition associated with increasing age and characterised by fusion of vertebral bodies and enthesopathies at the heel, elbow, iliac crest and other areas.
Nine individuals displayed enthesopathies. Areas affected include the insertion of the quadriceps into the patella (four individuals), the bicipital tuberosity of the radius, greater and/or lesser trochanters of the femur, obturator foramen, iliac crest, Achilles tendon insertion on the calcaneus, distal tibia/fibula articulation, insertion of triceps into ulna head (two individuals each), the ischial tuberosity, epicondyles of the humerus, coracoid process of the scapula (one individual each). In SK 252 the lesions around the distal tibia/fibula joint and other areas of the foot may be related to the separation of the tip of the distal fibula, reflecting trauma sustained at the time of the injury, or abnormal stresses caused as a consequence of the non-union. One old male may have suffered from DISH, displaying multiple enthesopathies [Photo 0514] and spinal fusion (SK 221).

Osteochondritis dessicans
Osteochondritis dessicans is a trauma-related condition of the joints, probably caused by an interruption of the blood supply to an area of bone and damage to the overlying cartilage. Osteochondritis dessicans is most common today in the knee in adolescent and young adult men engaged in strenuous physical activities such as football. It is manifest in the dry bone as a defect of the joint surface which may be lytic or proliferative, and may form a bony 'plug' which fills the defect and rises above the articular plane.
Perhaps surprisingly in view of the ample evidence for spinal stress in the present sample, only three possible examples of osteochondritis dessicans were noted. Two examples were in the elbow (SK 249, subadult possible male and SK 254, early middle-aged male) and one in the knee (SK 101, middle-aged possible male).
Defects of the articular surfaces
A characteristic defect of unknown aetiology, but possibly related to osteochondritis dessicans, was observed on a number of joint surfaces. The defect was characteristically lytic, varying from a minor depression in the articular surface to a lesion deep into the cancellous bone. The opposing joint surface was unaffected. The defect generally appears to be distinct from osteochondritis dessicans although some overlap may be noted (Cardy 1997a). Defects of the articular surfaces have been noted by many workers (various pers. comm.) but are not generally reported in the literature. Examples of the defect in the proximal phalanx of the great toe examined by a radiologist could not be detected on x-ray and were considered to be of no clinical significance (Dr D. Jones, pers. comm.). It may be significant that the bones most commonly affected are those along which the major transfer of weight occurs during locomotion, from the heel, through the first metatarsal and into the big toe. Whilst a developmental aetiology cannot be excluded, none of the defects follow lines of epiphyseal fusion, nor do they correspond to known sites of blood vessels.
Frequencies were recorded for the bones in which the defect was most common in the Whithorn sample (Cardy 1997a) (Table 31). These were the proximal facet of the first phalanx of the great toe, the talus facet of the navicular, the base of the first metatarsal and the superior facets of the second cervical vertebra.
The frequencies obtained for defects of the articular surfaces in this current population are low compared with other populations, the most striking difference being seen in the cervical vertebrae where there was a total absence of defects compared with 12% at St John's Tower, Ayr. Comparisons between west and east coast Scottish sites hint at higher frequencies on the west coast, although more comparative data is needed to examine this further.
Degenerative joint disease
Degenerative change at the joints (osteoarthritis) is the most common pathology seen in most skeletal collections. Degenerative joint disease is incompletely understood but is probably best explained by a multifactorial model in which age, trauma, endocrine agents, heredity, sex and diet all play a role (Jurmain 1977).
Two main types of degenerative joint disease are usually distinguished; primary osteoarthritis where the changes appear to reflect skeletal ageing, and secondary osteoarthritis when the changes reflect an alteration of the joint mechanics as when a fracture heals out of alignment. Primary degenerative joint disease is often generalised whereas secondary degenerative joint disease is usually limited to one joint. Primary degenerative joint disease was one of the 'ageing' criteria used in the present sample. It is difficult to give an accurate account of the frequency of degenerative joint disease because of the incompleteness of many of the remains. Frequencies of joints affected as a proportion of the number at risk are therefore not given although the relative amounts of degenerative joint disease in different areas is examined.
Forty adults showed some degenerative changes. The spine was involved most often, 25 individuals being affected in this area. The different regions of the spine were affected equally, although changes in the cervical spine tended to be more severe than elsewhere. Vertebral bodies were affected more often than the facet joints. Other regions affected in order of decreasing frequency were the wrist (15 individuals), elbow (14 individuals), knee (12 individuals), fingers and shoulder (11 individuals), hip (nine individuals), ankle (5 individuals) and toes (3 individuals). Degenerative changes were most severe in the wrist, especially in the distal ulna and first carpal row where five individuals displayed eburnation (see below).
Degenerative change was judged to be secondary in the proximal joint of the left first finger of SK 239 although the predisposing injury was not evident. Secondary degenerative joint disease was also present on the distal facet of a disarticulated radius with a fracture of that facet.
Severe degenerative joint disease may be associated with complete erosion of the articular cartilage leading to a polishing of the joint surfaces known as eburnation. Eburnation was noted in seven individuals including four males and two females. Most was seen in the wrist, four at the distal radius/ulna joints and one at the capitate/scaphoid joint, followed by the metatarsal heads (two individuals) and hip and cervical facet joints (one individual each). Left and right sides were equally affected.
Dislocation
One middle-aged female (SK 250) probably suffered from recurrent anterior/inferior dislocation of the right proximal humerus, the most common type of dislocation at this joint. A new articular surface had formed on the body of the scapula although the original articular surface appeared to be normal as did the humeral shaft. The small portion of the humeral head which survived was light and fragile and of abnormal morphology.
Periosteal new bone development
Direct trauma, infection, venous stasis (e.g. varicose veins) or muscle overuse may cause inflammation of the periosteal membrane which covers the non-articular surfaces of all bones, stimulating the membrane to produce new bone over the original bone surface. The new bone is initially largely separate from the original cortex but with time becomes remodelled and incorporated into the old bone surface.
As with other skeletal collections, the tibia and/or the fibula were the most frequent sites of periosteal new bone development and 56% (5/9) of all cases involved these bones. The medial surface of the tibia has very little subcutaneous protection making it vulnerable to traumatic injury although in some diseases (e.g. syphilis) new bone is preferentially deposited on the cooler bone surfaces such as the medial and lateral tibial surfaces.
A non-specific condition known as 'shin splints' is commonly recognised in the field of modern sports medicine. It is manifest as pain in the lower leg, usually in the distal third of the medial/posterior surfaces. It seems to represent a continuum from periosteal new bone at one extreme to stress fracture at the other and may be caused by active remodelling of the bone or by traction caused by muscle pull on the periosteum (Batt 1995). As medieval populations were probably subject to significant lower limb stress it seems reasonable to suggest than shin splints may account for a proportion of the periostitis seen in archaeological collections.
Infection is indicated if the bone/s displaying periosteal new bone development are well-protected by subcutaneous tissues, or if the involvement is extensive. Specific infections known to cause periosteal new bone development include typhoid fever, tuberculosis, syphilis, leprosy and hypertrophic pulmonary osteoarthropathy (e.g. bronchial carcinoma, bronchiectasis and metastatic tumours of the lungs) although the lesions themselves are rarely diagnostic of a particular condition (Anderson 1985).

Of the nine individuals displaying periosteal new bone development, the deposits in four cases were restricted to the lower leg indicating local causal mechanisms, systemic factors being implicated in the remaining cases. Deposits on the inner surface of the calvarium of the infant SK 224 [Photo 0501] may indicate meningitis; those on the pleural surface of the ribs of two adults (SK 213, SK 228) may indicate lung infection such as pneumonia or tuberculosis. The widespread, unhealed deposits on a female (SK 231, forearms, scapula, sacrum, possibly the femora, and the tibiae and fibulae affected) indicate systemic infection which was active at the time of death; those of the lower leg in SK 223 probably relate to leprosy infection or psoriatic arthropathy [Photo 0293].

Fifteen percent (31/211) (Table 32) of adult tibiae displayed periosteal new bone development. In most cases this was minor and healed. Periosteal new bone was most common on the medial surface (24/196, 12%), and least common on the posterior surface (17/205, 8%), the lateral surface being in an intermediate position (21/202, 10%). Although minor, the differences may reflect the amount of protection afforded to each bone surface by the overlying tissues and thus the vulnerablility of the periosteum to trauma.
Leprosy
Leprosy prevalence reached a peak in Europe around the time of the Crusades (1096-1221) but began to decline at the beginning of the Renaissance, possibly due to improved living conditions. Approximately 1% of a population may be infected with Mycobacterium leprae where leprosy is endemic, and of those approximately 15% will show skeletal changes. Bone changes are most common in lepromatous leprosy, the low resistance form of the disease (Steinbock 1976). Unfortunately the bones most often affected (the small bones of the hands and feet and the nasal area) survive relatively poorly in archaeological material and skeletal evidence of leprosy may therefore be sparse even in populations in which the disease was common.


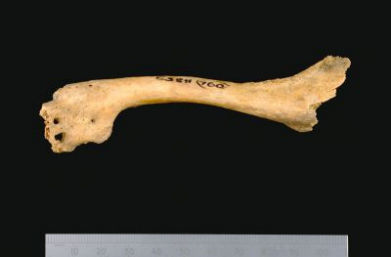
One possible example of leprosy was noted. SK 223 (mature male) displayed classic resorptive changes to the metatarsals and phalanges of the feet [Photo 0317], the affected bones being very fragile and osteoporotic. A number of the tarsals [Photo 0337] were fused together and with the metatarsals, probably as a consequence of soft tissue infection subsequent to nerve damage. Only one finger appears to have been affected, with fusion of the proximal and interproximal phalanges and resorption of the interproximal bone. There was also resorption and pitting of the maxilla [Photo 0417] with loss of the central incisors although the anterior nasal spine was unaffected. There was also fusion with kyphosis of the mid thoracic vertebrae (Pott's spine) which, although not pathognomic of tuberculosis, is often associated with the disease. Tuberculosis is often a fatal consequence of lepromatous leprosy. Significant periostitis was noted on the tibia and fibula [Photo 0293], a feature commonly associated with the disease.

Differential diagnoses include psoriatic arthropathy (arthritis related to psoriasis). Unfortunately the sacro-iliac joints and most of the spine, commonly involved in psoriatic spondyloarthropathy, were unavailable for study.
Tuberculosis

There were a number of examples of pathology consistent with a diagnosis of tuberculosis. The vertebral column of an 8-10 year old child (SK 26) [Photo 0202] displayed changes consistent with tuberculosis infection, as did that of an adult female (SK 100) with gross destruction of the vertebral bodies between the 7th and 10th thoracic vertebrae. The spinal changes in an adult male (SK 223) may reflect tuberculous infection superimposed on leprosy infection. In addition, a number of examples of infection, such as that of the sternum and clavicle may have been caused by tuberculosis.
Between 5% and 7% of those contracting tuberculosis develop bony changes, and of those 25% to 50% show the spinal features from which the disease is usually diagnosed (Steinbock 1976). This 'Pott's spine' is characterised by destruction and collapse of the anterior part of the vertebral bodies leading to kyphotic fusion (angulation giving the appearance of a hunched back), usually in the lower thoracic and/or lumbar region. Other large joints may be affected although the changes may be indistinguishable from septic arthritis and other severe joint conditions. The pulmonary form of tuberculosis may also cause deposition of new bone on the visceral surface of the ribs.

Two further individuals displayed periosteal new bone deposits on the inner surface of the ribs which indicate lung infection of some kind which may include tuberculosis. In addition, the pathology at the joint between the disarticulated clavicle [Photo 0132] (context A760) and manubrium [Photo 0392] (context A1218) indicates a septic arthritis which could be of tuberculous origin as this is a common site of tuberculous involvement.
Despite ample evidence of infection, the causal organism could be suggested in only one individual who may have suffered from both leprosy and tuberculosis (SK 223). Lung infection was implicated in two further cases with periosteal deposits on the pleural surface of the ribs. Typhoid fever, a disease associated with poor hygiene, may cause periosteal new bone development by haematogenous spread months or years after infection (Anderson 1985) and may account for some examples of periosteal new bone development. Other examples of periosteal new bone may have been caused by trauma including overuse.
Internet Archaeology is an open access journal based in the Department of Archaeology, University of York. Except where otherwise noted, content from this work may be used under the terms of the Creative Commons Attribution 3.0 (CC BY) Unported licence, which permits unrestricted use, distribution, and reproduction in any medium, provided that attribution to the author(s), the title of the work, the Internet Archaeology journal and the relevant URL/DOI are given.
Terms and Conditions | Legal Statements | Privacy Policy | Cookies Policy | Citing Internet Archaeology
Internet Archaeology content is preserved for the long term with the Archaeology Data Service. Help sustain and support open access publication by donating to our Open Access Archaeology Fund.